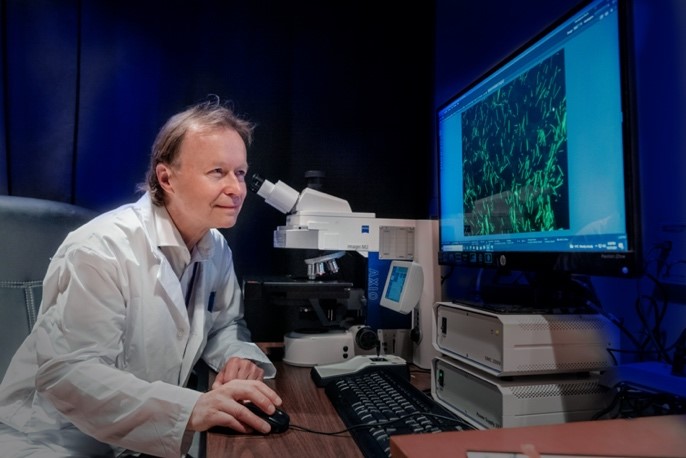
In this interview, we talk with Dr. Wolfram Tetzlaff, a co-investigator from the combination treatments team helping to realize the vision of Mend the Gap.
Tell us about yourself!
I completed my MD in Germany and my PhD in Calgary, which was followed by faculty appointments at the Universities of Calgary, Ottawa and finally, the University of British Columbia (UBC) where I hold the John and Penny Ryan BC Leadership Chair in Spinal Cord Injury Research. I serve as the Director of ICORD, the International Collaboration on Repair Discoveries, and lead a research program focusing on experimental strategies for neuroprotection and neural repair after spinal cord injury (SCI). In particular, my group found that fasting and diets affect the cascades of secondary damage after SCI and can improve outcomes. My group also works on axonal regeneration and cell transplantation, and demonstrated that skin-derived Schwann cells can be used for neural repair in the chronically injured spinal cord of animals. More recently, my group’s focus has been on the role of certain subtypes of cells within the central nervous system that are involved in spontaneous repair and remyelination after SCI.
What are the major challenges facing regeneration of the injured spinal cord?
The spinal cord contains millions of nerve fibres that connect the brain to the rest of the body. Most, if not all of these nerve fibres are severed at the site of a SCI, leading to paralysis of the body below the level of injury. In order to restore neural impulses across the lesion site, these nerve fibres have to regrow from the lesion edge across the lesion. Unfortunately, the cells at the lesion edge form a scar, and the lesion itself forms a fluid-filled cavity that can be centimeters long in humans. In addition, the growth propensity of the nerve cells in the brain is limited.
Basic research over the past decade has provided us with some understanding of how molecular mechanisms at the site of injury prevent nerve fibre growth. Based on some promising data in animals, several treatments aiming to overcome these inhibitors with certain drugs, compounds, or even cells, are currently in or preparing for trials in humans; however, there has been no successful trial yet. There is still a long path from seeing success in small animals to achieving success in humans. Neural stimulation and neuro-prosthetics are a parallel approach that either augments the function of a few spared nerve fibres or that uses electrical commands from the brain to drive limb movements. Both approaches will likely merge in the future, since we can only regenerate a fraction of the severed nerve fibres, and these need to be trained and augmented by electrical stimulation and rehabilitation training. Rehabilitation training after surgical stabilization is currently the only validated treatment option after injury.
How will Mend the Gap seek to meet this challenge?
First and foremost, Mend the Gap seeks to build a bridge by using smart biomaterials which can be injected into the lesion site where they can be aligned to support nerve fiber regeneration across the site of injury. Injections into the spinal cord are well tolerated and by using a gel-like material, these bridges can fill and follow the shape of the lesions that are different in every person. In order to enhance effectiveness, the bridges will carry molecules and release drugs that enhance nerve fibre growth and neutralize the growth inhibitors in the scar. Stimulation of growth and training will be addressed by novel neuromodulation approaches.
What is your long-term vision for treating spinal cord injury?
Ideally, the result of this project will be that we have developed an injectable, alignable biomaterial platform, which can be combined with further co-treatments that are already approved by regulatory agencies as drugs for other applications. This strategy would be demonstrated to work in small and large animals, providing sufficient evidence to move towards human trials. The engineers on our team will develop novel, robotic, image-guided injection methods to translate such an approach to the clinic. The biomaterial platform will be widely available to other researchers, who can use it to test their own “magic bullet” co-treatment, which may address specific types of injuries and create a more personalized approach to treatment. Our guiding principle is to improve treatment without sacrificing the gains that may be seen in patients over the first year of healing – safety is therefore our top priority.
Where does your passion come from?
I have been fascinated by nerve injury since I was a child due to a case in my family. Seeing the immense challenges that people with neural injury face, in particular with SCI, brought me into Medicine and subsequently Neuroscience. Spinal cord regeneration is still the holy grail of neuroscience. Being part of such an effort like Mend the Gap is a formidable opportunity to push these frontiers.